INTRODUCTION
Nocardia species are aerobic, Gram-positive, beaded, weakly acid-fast, branching rods. Nocardiosis results from infection by members of the genus Nocardia, which are ubiquitous environmental saprophytes that cause localized or disseminated diseases in humans via inhalation or inoculation [
1]. Immunocompromised individuals with deficient cell-mediated immunity, especially that associated with lymphoma, transplantation, glucocorticoid therapy, or human immunodeficiency virus infection, are at risk for Nocardiosis [
2]. Pneumonia is the most common form of Nocardia disease, and other common sites include the brain, skin and soft tissues, kidneys, joints, bones, and eyes [
1-
3]. Muscle involvement is rare and a typical manifestation of muscle infection is a subacute intramuscular abscess [
4]. Here, we present a rare case of rapidly progressive multifocal intramuscular abscesses caused by
Nocardia abscessus identified by matrix-assisted laser desorption/ionization time-of-flight mass spectrometry (MALDI-TOF MS).
CASE REPORT
A 73-year-old man presented to the emergency department with progressive back pain and pain radiating down the left leg that had worsened over the past 25 days. He also reported fever and chills. His medical history included chronic obstructive lung disease (COPD) treated with home O2 therapy, prednisolone 5 mg/day, and montelukast sodium 10 mg/day. He had received an epidural nerve block 3 days previously.
On admission, he had a temperature of 38.7в„ғ, heart rate of 120 beats/min, and blood pressure of 87/56 mmHg. His oxygen saturation was 88% while breathing ambient air. Physical examination revealed decreased sounds in both lungs and severe tenderness of the buttocks and left thigh. The motor and sensory functions of both legs were intact. Laboratory tests revealed a white blood cell count of 45.7/ВөL, hemoglobin of 12.1 g/dL, platelet count of 407.0 Г— 103/ОјL, C-reactive protein level of 22.5 mg/dL (normal range, 0-0.5), procalcitonin level of 8.9 ng/mL, and lactic acid level of 3.0 mmol/L. Three sets of blood cultures on blood agar and MacConkey agar plates for 5 days were negative.
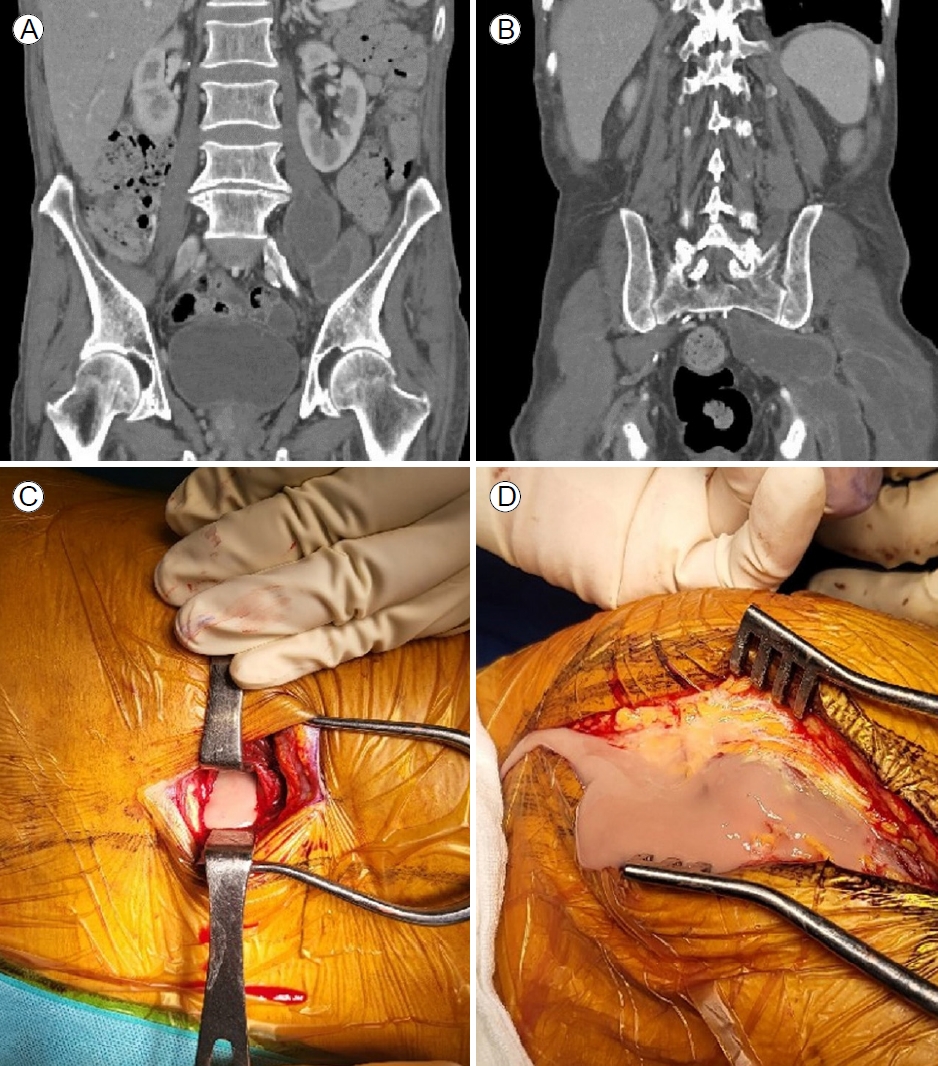
On the first day of admission, chest radiography and chest and abdominopelvic computed tomography (CT) showed extensive emphysema with chronic bronchitis, and revealed extensive intramuscular abscesses involving the left psoas, iliacus, spinalis thoracis, longissimus thoracis, gluteus maximus, and piriformis muscles (
Fig. 1A, B). On the fourth day after admission, the pain in the left hip and thigh worsened despite the administration of broad-spectrum antibiotics (levofloxacin and vancomycin) and analgesics. Lumbar spine CT revealed a combined anterior epidural abscess at the L4 to S1 levels and suggested bony involvement of the left sacrum and lower lumbar spine. On the sixth day after admission, incision and pus drainage of the left iliopsoas, gluteal, and paravertebral abscesses were done to relieve pain and as definitive treatment. Yellow and brown pus was released from the psoas, iliacus, and paraspinal muscles (
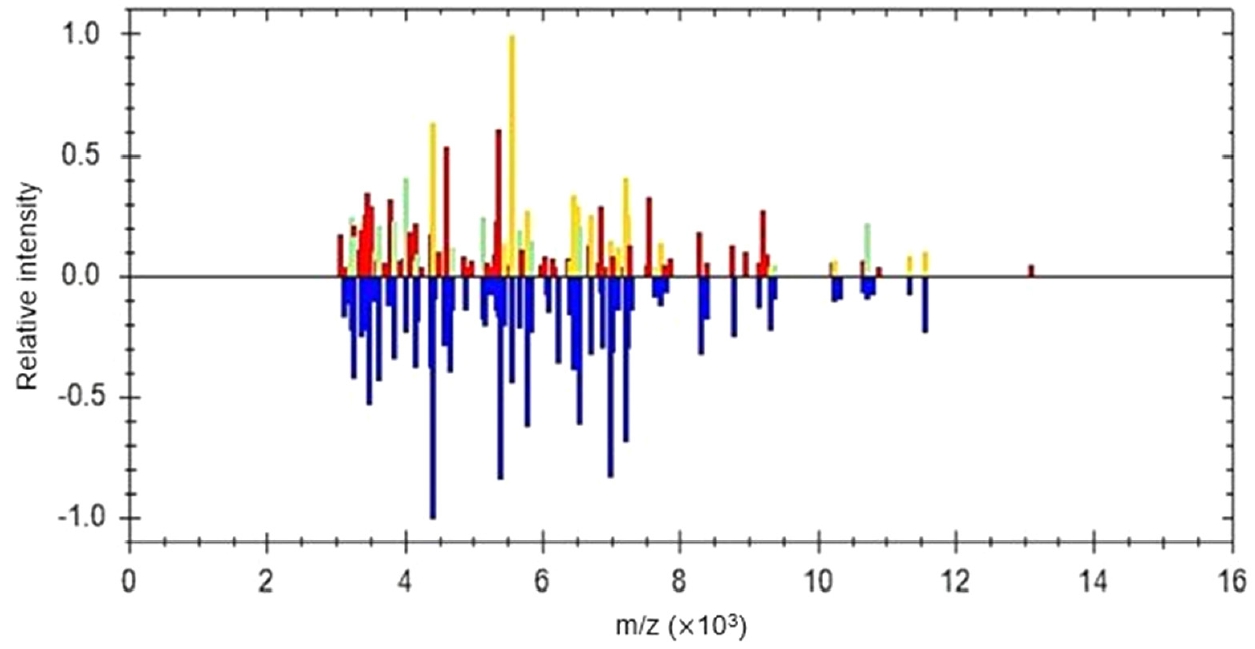
Fig. 1C, D). The psoas and paraspinal muscle histopathology showed many acute inflammatory cells with macrophages in a necrotic background. Gram stain and culture of pus and tissue specimens from the psoas, iliacus, and paraspinal muscles and Gram staining of surgical specimens initially showed no bacteria, but after 2 days incubation, Gram-positive filamentous rods were observed on Gram staining of cultured colonies. Four hours after the colonies were grown, the bacteria were identified as
Nocardia abscessus using MALDI-TOF MS (
Fig. 2). On the eighth day after admission, the acute exacerbation of COPD continued to progress, despite mechanical ventilation and the administration of high-dose steroids, and the patient died.
DISCUSSION
The organs most frequently infected by Nocardia are the respiratory tract, brain, and skin/soft tissues [
1-
3]. Intramuscular nocardiosis is rare; to our knowledge, only 15 cases have been reported (
Table 1), including six cases each of
Nocardia asteroids (N. asteroids) and
Nocardia farcinica [
5-
8]. The psoas is the most common site of intramuscular infection due to its rich vascular nature, and a secondary psoas abscess may occur as local spread from the viscera along the iliopsoas. In an analysis of 93 psoas abscesses for which the causative microorganisms were identified over 15 years [
9], there was one case of
Nocardia (
N. asteroides). In a literature review (
Table 1), in 6/15 (40%) of cases, the muscle was the primary site of infection; in 9/15 (60%) of cases, multiple organs such as lung, brain, bone, and spleen were co-infected. Most (13/15 cases; 87%) patients were immunocompromised and three patients (cases 3, 5, and 6), including an immunocompetent patient, had jobs with a risk of
Nocardia inhalation or inoculation. In our case, although 5 mg/day prednisolone is not an immunosuppressive dose, inhalation might have been a route of Nocardia infection, considering the patientвҖҷs very severe COPD with home O2 therapy and bed-ridden state.The organs most frequently infected by Nocardia are the respiratory tract, brain, and skin/soft tissues [
1-
3]. Intramuscular nocardiosis is rare; to our knowledge, only 15 cases have been reported (
Table 1), including six cases each of
Nocardia asteroids (N. asteroids) and Nocardia farcinica [
5-
8]. The psoas is the most common site of intramuscular infection due to its rich vascular nature, and a secondary psoas abscess may occur as local spread from the viscera along the iliopsoas. In an analysis of 93 psoas abscesses for which the causative microorganisms were identified over 15 years [
9], there was one case of Nocardia (N. asteroides). In a literature review (
Table 1), in 6/15 (40%) of cases, the muscle was the primary site of infection; in 9/15 (60%) of cases, multiple organs such as lung, brain, bone, and spleen were co-infected. Most (13/15 cases; 87%) patients were immunocompromised and three patients (cases 3, 5, and 6), including an immunocompetent patient, had jobs with a risk of Nocardia inhalation or inoculation. In our case, although 5 mg/day prednisolone is not an immunosuppressive dose, inhalation might have been a route of Nocardia infection, considering the patientвҖҷs very severe COPD with home O2 therapy and bed-ridden state.
As empirical antibiotics for typical intramuscular abscesses are not effective for abscesses caused by
Nocardia species, identification and antibiotic susceptibility tests followed by culture should not be delayed. Since
Nocardia has a low blood culture detection rate of 38% and a median incubation time of 4 days [
10], incision and drainage should be performed to obtain samples as soon as possible. As intramuscular abscesses are usually subacute, there was usually sufficient time to identify the
Nocardia species and prescribe specific antibiotics in most of the reported cases (
Table 1). However, our patient had an acute manifestation of Nocardiosis and died before the final culture results were available. Although only 2 days were taken to identify the
Nocardia abscessus (
N. abscessus), incision and drainage were delayed due to the patientвҖҷs unstable general condition and were performed after the sixth day of hospitalization. Empirical antibiotics for intramuscular abscesses, such as levofloxacin and vancomycin, ultimately proved ineffective. Case 1 in the literature review (
Table 1), was lost to follow-up after using penicillin without microbial identification and died 3 months later due to dissemination. We suspected
Nocardia in that case because filamentous shapes were observed on Gram staining. The differential diagnosis of Gram-positive rods includes
Corynebacterium, Listeria, Lactobacillus, Actinomyces (mainly as bacterial contaminants), and
Nocardia species. If the Gram-positive rods are filamentous,
Nocardia should be considered. Moreover, if staining for acid-fast bacilli reveals specific aerial hyphae, it helps to confirm
Nocardia [
1]. If cultured, Nocardia can be identified accurately using MALDI-TOF MS or 16S rRNA sequencing [
1-
3]. MALDI-TOF MS is used more commonly, owing to its short time and ease of use compared with 16S rRNA sequencing. The concordance between MALDI-TOF MS and 16S rRNA sequencing at the species/complex level is 97.3% [
3].
The 2019 updated guidelines for
Nocardia infection [
10] recommended that the initial selection of an antimicrobial regimen be based on the
Nocardia species.
N. abscessus is generally susceptible to trimethoprim/sulfamethoxazole (TMP/SMX), amikacin, ceftriaxone, amoxicillin-clavulanic acid, tigecycline, variably susceptible to imipenem and minocycline, and resistant to ciprofloxacin, moxifloxacin, and clarithromycin/azithromycin. However, in an analysis over 10 years conducted in Spain [
2], 2.8% and 4.2% of
N. abscessus isolates were resistant to TMP/SMX and amoxicillin-clavulanic acid, respectively.
In summary, this case of multifocal intramuscular abscess caused by
N. abscessus has educational value. Although the incidence of nocardiosis is increasing globally [
10], intramuscular abscesses are still uncommon. This case highlights the importance of considering the possibility of
Nocardia in patients with muscle abscesses and the value of using molecular techniques for identifying
Nocardia.





 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print




