INTRODUCTION
Despite pruritus being a very common symptom, doctors, except dermatologists, usually do not pay much attention to itching. However, many patients suffer from itching, which is often associated with systemic diseases such as diabetes mellitus (DM), chronic kidney disease (CKD), liver cirrhosis, malignancy, rheumatoid disease. and acquired perforating dermatosis (APD). The latter condition induces intense pruritus mainly in patients with DM and CKD. No definitive treatment is available and it can be difficult to cure.
Antihistamines or topical steroids can be used to treat APD, followed by phototherapy and oral isotretinoin in cases showing severe symptoms. Dermatologists concerned about impaired renal function and unexpected adverse reactions have no treatment options for CKD patients. Thus, cooperation between the dermatologist and nephrologist is important for optimal treatment of APD in CKD patients.
This report describes peritoneal dialysis (PD) in a patient with APD who was successfully treated using oral isotretinoin. In the past, he had been received all available treatments, including topical steroids, phototherapy, topical isotretinoin, and immunosuppressants; however, they all proved ineffective.
CASE REPORT
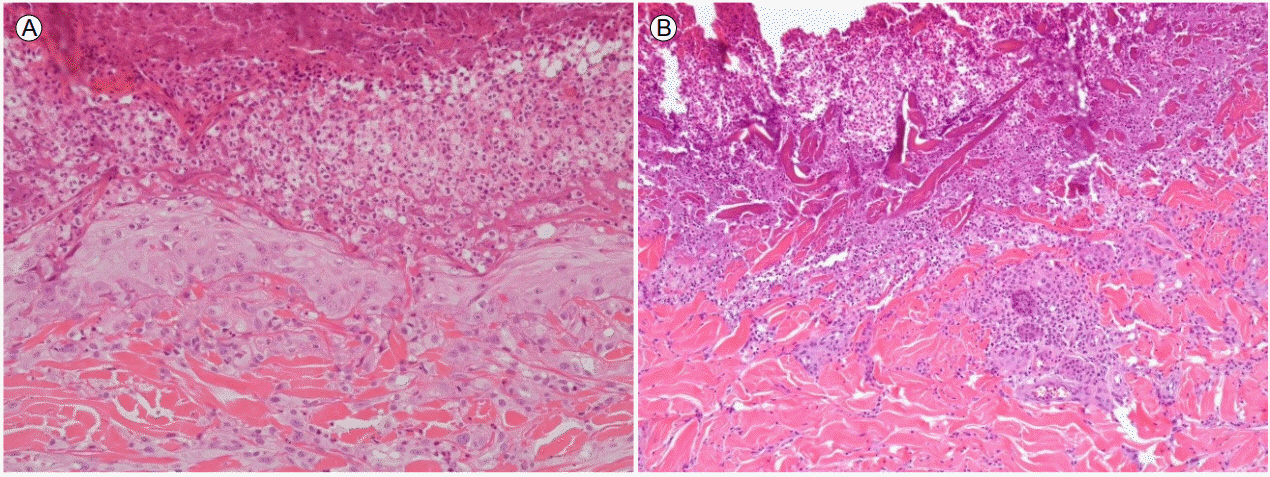
A 68-year-old man suffering from DM and end-stage renal disease, and who was undergoing PD, was admitted to the nephrology department complaining of painful skin lesions with severe pruritus. Because of the intense pruritus (visual analog scale score = 10), he could not sleep well, and everyday life became impossible. A physical examination revealed multiple, round, umbilicated, erythematous papules, and nodules with a central keratotic plug distributed over the entire body (Fig. 1). Initial laboratory results were as follows: white blood cells (WBCs), 9,500/mm3; C-reactive protein, 20 mg/L; hemoglobin A1c, 7.5%; calcium, 8.6 mg/dL; phosphorus, 4.3 mg/dL; and parathyroid hormone (intact), 155 pg/mL. His continuous ambulatory PD regimen included three 1.5% glucose exchanges and one icodextrin dialysis (8-hour dwell time). A skin biopsy was performed for definitive diagnosis after consultation with a dermatologist. The pathological report revealed inflammatory cells above the umbilicated lesions. Transepidermal collagen was absent (Fig. 2). Based on the clinical manifestations and biopsy results, the patient was confirmed to have APD.
Topical steroids, topical isotretinoin, and narrow-band ultraviolet B (UVB) phototherapy were applied but proved ineffective. He was taking allopurinol, which is another APD treatment, for control of gout. As the pruritus had not improved, we recommended hemodialysis as a potentially beneficial APD treatment, but he refused. Finally, oral isotretinoin was used.
Remarkable improvement of symptoms was observed 3 days after 10 mg/day oral isotretinoin. The lesions had disappeared 1 week after the oral isotretinoin, and only scars remained. There were no side effects except a dry mouth. Oral isotretinoin (10 mg/day) was taken every other day after the skin lesions had improved and was stopped completely 2 months later; there was no recurrence.
DISCUSSION
APD is an uncommon dermatological disease, and so is not a major concern of internal medicine departments even though it is closely associated with systemic disease. However, when APD occurs in a patient with CKD or DM, the treatment choices are limited due to concerns regarding impaired renal function and unexpected side effects. Thus, systemic agents tend to be used less frequently in patients with CKD and DM [1,2].
APD is different from perforating disease, which is not related to any specific medical condition. Perforating disease is divided into four types based on the pathological features. However, there are no recognized APD subtypes. Our patient was diagnosed with APD based on a biopsy and the clinical history. Although the pathogenesis of APD is unclear, the following etiologies have been proposed: 1) epidermal or dermal abnormalities due to alterations in the elastic fibers and collagen, possibly due to metabolic disorders caused by CKD 2) microdeposition of byproducts, such as calcium, uric acid, and hydroxyapatite, caused by CKD. 3) Diabetic vasculopathy, which is a major predisposing factor in patients with DM who scratch their skin. Trauma, including scratching, causes dermal necrosis, which is attributable to the poor blood supply associated with DM vasculopathy; this necrotic dermal material pushes out the epidermis [3]. As the pathological mechanism has not been defined, there is no gold standard therapy for APD.
Currently available treatments include UVB phototherapy and psoralen combined with ultraviolet A (PUVA), allopurinol, oral or topical retinoids, and topical steroids [4-6]. Despite the availability of these treatment modalities, only topical retinoids, topical steroids, and UVB phototherapy are typically used. Regarding the use of oral isotretinoin in CKD patients, it should be noted that Isotretinoin is a fat-soluble vitamin A derivative. For this reason, there are concerns about accumulation and side-effects in these patients. Previously, four APD patients were treated successfully with oral isotretinoin, but none had renal impairment. This is the first reported case of a PD patient treated using oral isotretinoin. In another study, nodulocystic acne improved with oral isotretinoin in hemodialysis patients, with no significant adverse reactions [7].
The mechanism of action of isotretinoin as a treatment for APD is unclear; however, an anti-inflammatory effect and induction of cell apoptosis have been suggested [6,8]. Careful monitoring is essential, as there is little evidence that the drug has been used in advanced CKD and dialysis patients. Commonly known adverse reactions of isotretinoin include teratogenicity and mood changes, mucocutaneous problems, increased liver enzyme levels, and allergic reaction. In this case, the patient presented with dry mouth, a temporary mood change, and aggressive behavior, which soon abated.
In the present case of PD, we used all known APD treatments, including topical steroids, topical retinoic acid, allopurinol, and phototherapy, but none produced a response. However, the patient showed significant improvement after the administration of oral isotretinoin.
Although there is a high incidence of APD among DM and CKD patients, internal medicine physicians have limited knowledge and experience with this entity. Systemic diseases, such as DM and CKD, can make it more difficult for dermatologists to select the optimal medications.
Previous reports about APD were mostly by dermatologists or pathologists, and thus naturally took a dermatological or pathological perspective. We hope that this report is instructive regarding how to treat refractory APD in a CKD patient using oral isotretinoin.




 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print






