 |
 |
| Korean J Med > Volume 99(4); 2024 > Article |
|
Abstract
Emphysematous prostatitis with an abscess is an extremely rare but lethal infection, characterized by the accumulation of gas and purulent exudates. Due to its rarity, severity, and nonspecific presentation, prompt diagnosis and treatment are crucial to achieve favorable clinical outcomes. This report presents a 43-year-old male with hemodialysis-dependent end-stage kidney disease who reported a 3-day history of fever, urinary incontinence, dysuria, and dyspnea. His condition rapidly deteriorated due to septic shock caused by emphysematous prostatitis with an abscess. Following extensive treatment including long-term parenteral antibiotics, polymyxin B hemoperfusion filter treatment, abscess drainage via transurethral resection of the prostate, and suprapubic cystostomy, the patient successfully recovered.
Emphysematous prostatitis with an abscess is a rare but potentially life-threatening infection characterized by the accumulation of gas and purulent exudates within the prostate. According to previous studies, the mortality rate ranges from 3% to 25% [1,2]. Known risk factors include immunocompromised status, diabetes mellitus, end-stage kidney disease (ESKD) requiring hemodialysis, liver cirrhosis, alcoholism, and recent urethral manipulation. There are few case reports of emphysematous prostatitis in hemodialysis-dependent patients with ESKD.
A 43-year-old male with a history of ESKD and diabetes requiring hemodialysis presented to the nephrology department. In 2022, he underwent wound debridement and left fifth metatarsal head resection due to a diabetic foot ulcer. He reported a 3-day history of dysuria, urinary incontinence, fever, and dyspnea. Despite being oliguric with urine output ranging from 50-350 mL/day and undergoing hemodialysis for 2 years, he had slightly preserved residual renal function. Upon presentation, his vital signs were blood pressure 100/50 mmHg, pulse 118 beats/min, respiratory rate 24 breaths/min, and temperature 38.8Ōäā. He appeared alert but acutely ill, exhibiting high fever and tachypnea, with coarse rales audible in both lungs. No costovertebral angle tenderness was noted, and a digital rectal examination showed no abnormalities. His oxygen saturation was 92% at 3 L/min via nasal cannula.
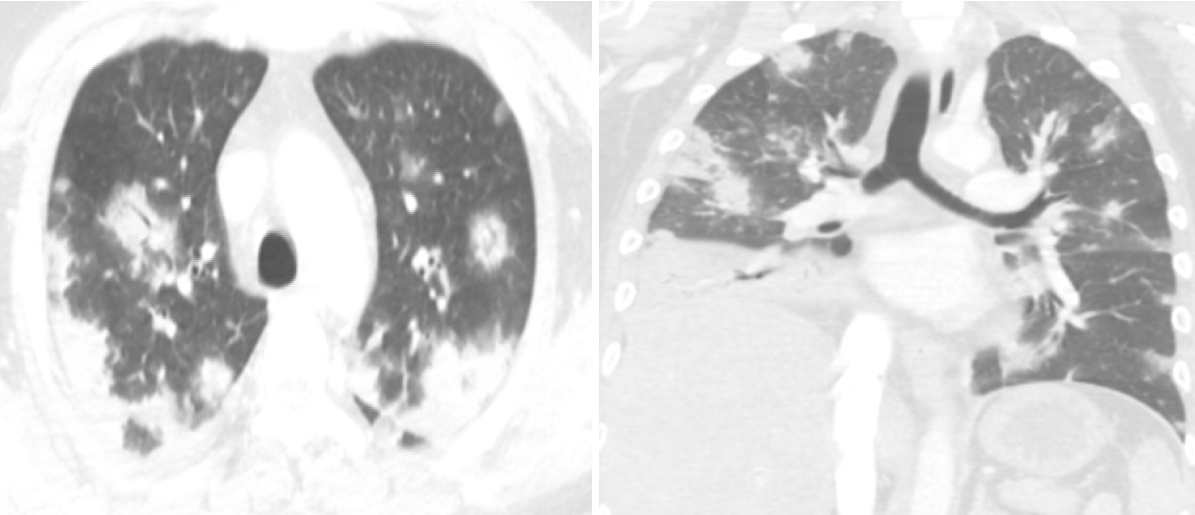
Laboratory findings revealed a white blood cell (WBC) count of 13,500/mm3, hemoglobin 9.5 g/dL, platelet count 207,000/mm3, C-reactive protein (CRP) level 22.91 mg/dL, procalcitonin > 100 ng/mL, blood urea nitrogen 44.7 mg/dL, serum level of creatinine 10.03 mg/dL, total CO2 content 24.4 mmol/L, random blood glucose 719 mg/dL, and hemoglobin A1C 8.0%. Routine urinalysis showed bloody and turbid urine with > 100 red blood cells per high power field (HPF), 31-50 WBCs/HPF, and mild bacteriuria. Initial plain radiography revealed multiple focal opacities in both lung fields and foci of air accumulation behind the pubic ramus. A subsequent abdominal computed tomography (CT) scan displayed multiple air foci in the prostate gland and bilateral seminal vesicles, with thickened urinary bladder walls indicative of emphysematous prostatitis with cystitis (Fig. 1). A chest CT scan demonstrated multifocal consolidations and groundglass opacities, likely due to septic embolic pneumonia (Fig. 2).
Ceftriaxone was administered intravenously along with fluid supplements following blood culture collection. By hospital day 3, the patientŌĆÖs condition deteriorated into septic shock, evidenced by a drop in blood pressure to 70/40 mmHg, WBC count of 8,550/mm3, hemoglobin level 8.6 g/dL, platelet count 44,000 mm3, CRP level 33.03 mg/dL, procalcitonin > 100 ng/mL, and interleukin-6 > 5,000.0 pg/mL. Arterial blood gas analysis indicated metabolic acidosis with lactic acidosis (pH, 7.157; HCOŌéā, 15.2 mmol/L; lactic acid, 5.0 mmol/L).
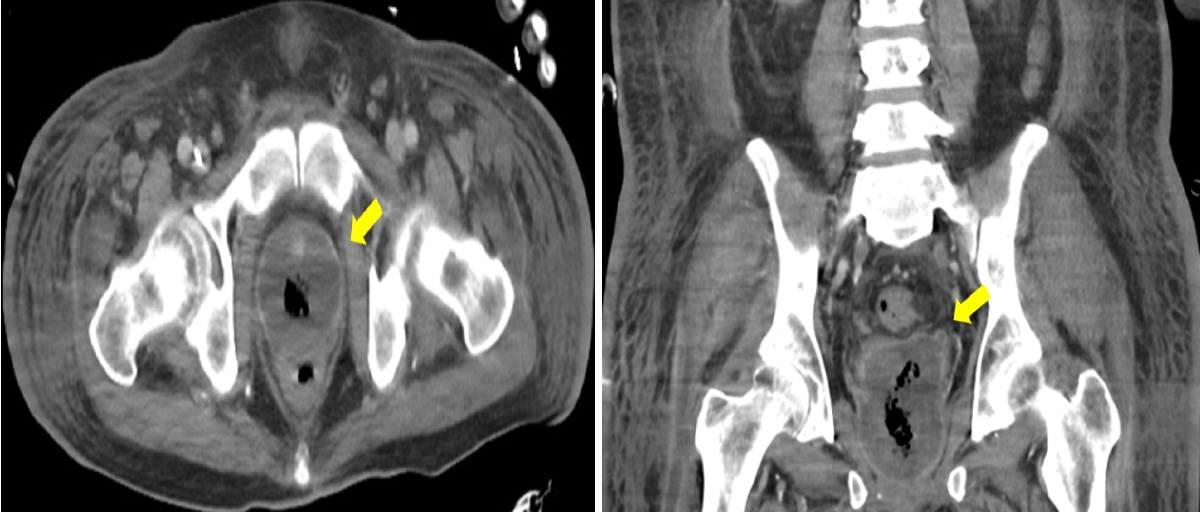
The patient was transferred to the intensive care unit (ICU) for further management as his septic shock worsened and respiratory compensation for metabolic acidosis was inadequate. Upon arrival in the ICU, he was intubated and placed on mechanical ventilation. Due to the apparent lack of infection control, a broader antibiotic regimen, specifically meropenem, was initiated. In addition, treatment with a polymyxin B-immobilized hemoperfusion filter (PMX-HP) was started for endotoxin removal, along with continuous renal replacement therapy (CRRT). An emergency urethral indwelling catheter was inserted to manage the retained urine and ongoing hematuria resulting from thrombocytopenia. One week later, the patient began to recover from septic shock and was successfully weaned off CRRT. Initial blood cultures had isolated extended-spectrum beta-lactamase negative Klebsiella pneumoniae; however, the antibiotic regimen was maintained due to the patientŌĆÖs severe septic condition. In the second week of admission, the patient underwent a suprapubic cystostomy and removal of the indwelling catheter for urinary diversion. On hospital day 18, he was successfully extubated. A follow-up abdominal CT scan showed that the prostate gland was replaced with an abscess, indicated by a peripheral enhancing low-attenuation lesion with a maximum diameter (Dmax) of 8.2 cm in the coronal plane (Fig. 3).
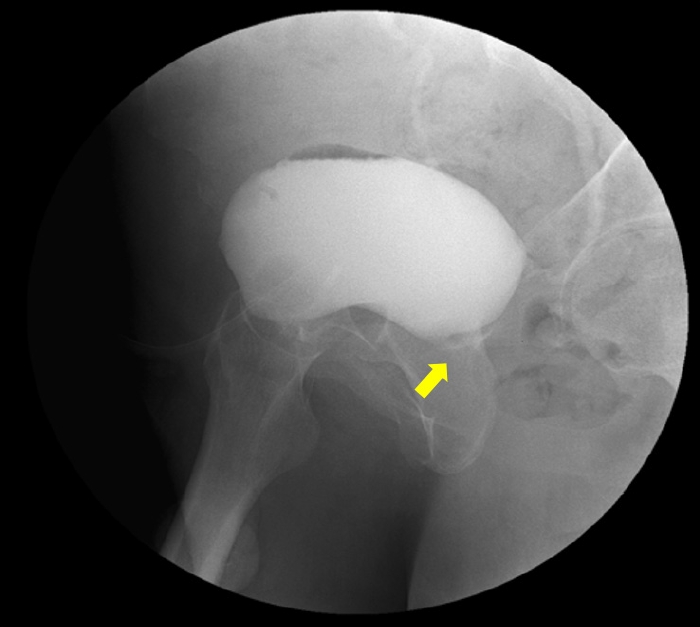
After his transfer to the general ward, he experienced recurrent fevers with elevated inflammatory markers, suggesting that the prostate infection with the abscess was not fully controlled. Consequently, the patient underwent transurethral drainage of the prostate abscess 1 month after admission. He gradually recovered post-surgery and received targeted parenteral antibiotics for 12 weeks based on the pathogens isolated from the initial blood cultures. He was discharged from the hospital with a cystostomy tube in place after discontinuing antibiotics and having no fever for 2 weeks. Subsequent abdominal CT scans showed a reduction in the size of the prostate abscess (Dmax, 5.4 cm). Thereafter the cystostomy tube was changed monthly due to the risk of urinary retention, as indicated by cystography showing a completely obstructed urethra (Fig. 4).
Emphysematous prostatitis with an abscess is a rare but potentially lethal infection, with mortality rates ranging from 3% to 25% [1,2]. Notable risk factors include immunocompromised status, diabetes mellitus, liver cirrhosis, alcoholism, urethral instrumentation, and the need for hemodialysis [3]. Patients with ESKD who are hemodialysis-dependent often experience oliguria or anuria, leading to bladder dysfunction and inadequate urine washout [4,5]. This condition predisposes retained urine to reflux of infectious pathogens, increasing the risk for severe infections. Prostatic abscesses are rare, with an incidence of 0.5%, and are challenging to differentiate from other urinary tract infections based on clinical symptoms alone, which makes their diagnosis difficult [6]. A comprehensive clinical history, thorough physical examination, and appropriate imaging modalities such as ultrasound and CT are crucial for diagnosis [7,8]. Broadspectrum parenteral antibiotics that cover Gram-negative bacteria are essential for treating prostatic abscesses [2,9]. Abscess drainage may be necessary when the infection does not respond to pharmacotherapy, performed either surgically or through minimally invasive methods such as transrectal, transperineal, or transurethral routes. If the abscess is < 1 cm in diameter, medical therapy alone may suffice. However, larger abscesses typically require prioritization of drainage procedures [10]. In addition, patients with voiding disturbances, such as urinary retention, may need urinary diversion [9-11]. An indwelling urethral catheter or suprapubic cystostomy can reroute retained urine. A suprapubic cystostomy is preferred for reducing intraprostatic pressure and preventing ductal reflux of urine, as it is less likely to cause ascending urethral infections compared to indwelling urethral catheters [2,12].
This report presents a hemodialysis-dependent patient with ESKD who developed emphysematous prostatitis with an abscess. Despite 3 weeks of targeted parenteral antibiotics based on pathogens isolated from blood and urine cultures, the infection was not fully controlled. Consequently, the abscess was drained via the transurethral route. Due to the patientŌĆÖs dysfunctional urinary bladder, retained urine refluxed back to the prostate, impeding recovery. To manage this, urine was rerouted via emergent indwelling catheterization, as the patientŌĆÖs thrombocytopenia with coagulopathy limited the use of more invasive procedures. Once the patientŌĆÖs bleeding tendency improved during the second week of admission, a suprapubic cystostomy was performed and the indwelling catheter was removed. In addition, PMX-HP therapy was initiated to manage severe sepsis caused by Gramnegative rod-shaped bacteria [13]. A PMX-HP filter, an adsorbent column that removes endotoxins including outer membrane components of Gram-negative bacteria, improves mortality rates in septic patients [13,14].
Patients with ESKD are predisposed to more frequent and severe infections than the general population, particularly with urinary tract infections, due to difficulties in collecting urine samples from those in an anuric or oliguric state. They also experience compromised immune function, reduced bladder activity, a higher prevalence of multidrug-resistant organisms, and often have comorbidities, which complicate diagnosis and treatment [15]. In this case, the de-functionalization of the urinary bladder in a patient undergoing dialysis for ESKD and a history of diabetes mellitus were significant risk factors for the development of emphysematous prostatitis. Given the rarity and potential lethality of emphysematous prostatitis with an abscess, timely diagnosis and treatment are crucial. Proper imaging modalities are essential for accurate diagnosis. Once diagnosed, treatment with parenteral antibiotics, with or without abscess drainage, is vital. Considering the typical urinary de-functionalization in ESKD, which may exacerbate infections, urinary diversion, such as cystostomy, is advisable to minimize the reflux of infected urine. Furthermore, PMX-HP filter therapy can be beneficial for managing uncontrolled sepsis, as demonstrated in this patient.
REFERENCES
1. Madani A, Chaker K, Trigui M, Ouanes Y, Azouz E, Nouira Y. Isolated emphysematous prostatitis: a very rare entity. Urol Case Rep 2023;49:102448.



2. Wen SC, Juan YS, Wang CJ, et al. Emphysematous prostatic abscess: case series study and review. Int J Infect Dis 2012;16:e344ŌĆōe349.


3. Brede CM, Shoskes DA. The etiology and management of acute prostatitis. Nat Rev Urol 2011;8:207ŌĆō212.


4. Stafford P, Prybys KM. Pyocystis and prostate abscess in a hemodialysis patient in the emergency department. West J Emerg Med 2014;15:655ŌĆō658.



5. Bibb JL, Servilla KS, Gibel LJ, et al. Pyocystis in patients on chronic dialysis. A potentially misdiagnosed syndrome. Int Urol Nephrol 2002;34:415ŌĆō418.


6. Reddivari AKR, Mehta P. Prostatic abscess. Treasure Island (FL): StatPearls Publishing, 2023.
7. Kuo PH, Huang KH, Lee CW, Lee WJ, Chen SJ, Liu KL. Emphysematous prostatitis caused by Klebsiella pneumoniae. J Formos Med Assoc 2007;106:74ŌĆō77.


8. Bae GB, Kim SW, Shin BC, et al. Emphysematous prostatic abscess due to Klebsiella pneumoniae: report of a case and review of the literature. J Korean Med Sci 2003;18:758ŌĆō760.



9. Mayouf S, Fourati M, Bchir S, Kammoun O, Mseddi MA, Slimen MH. Emphysematous prostatitis: a case report. Urol Case Rep 2020;34:101459.



10. Abdelmoteleb H, Rashed F, Hawary A. Management of prostate abscess in the absence of guidelines. Int Braz J Urol 2017;43:835ŌĆō840.



11. Lee DS, Choe HS, Kim HY, et al. Acute bacterial prostatitis and abscess formation. BMC Urol 2016;16:38.



12. Yoon BI, Kim S, Han DS, et al. Acute bacterial prostatitis: how to prevent and manage chronic infection? J Infect Chemother 2012;18:444ŌĆō450.


13. Mitaka C, Tomita M. Polymyxin B-immobilized fiber column hemoperfusion therapy for septic shock. Shock 2011;36:332ŌĆō338.


Abdomen-pelvis CT obtained upon admission shows multiple air foci in the prostate gland and bilateral seminal vesicles (arrows), indicating emphysematous prostatitis with an abscess. CT, computed tomography.
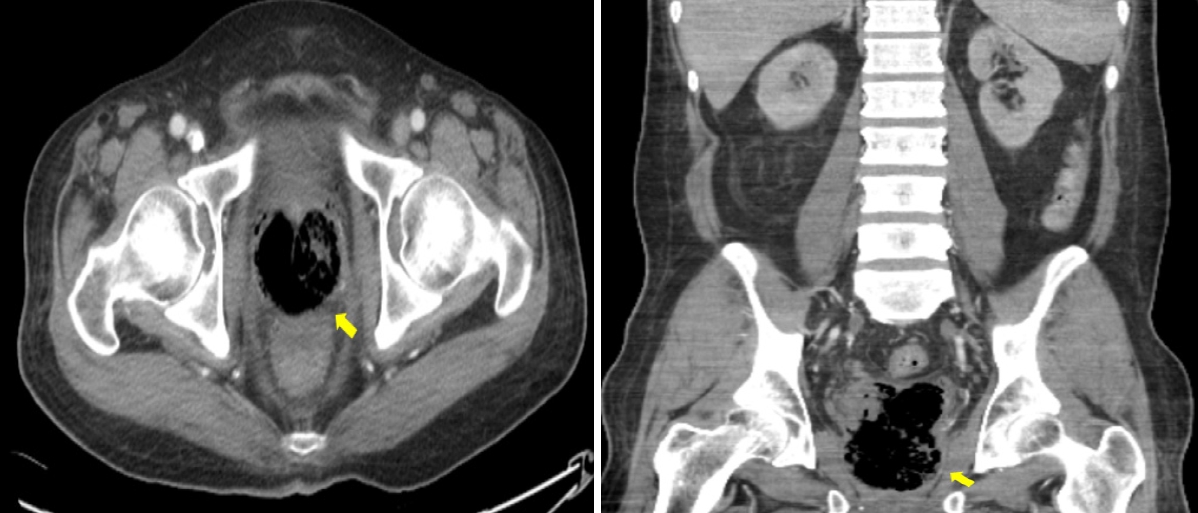
Figure┬Ā1.
Chest CT obtained upon admission reveals multifocal ground-glass opacities and consolidations in both lung fields, consistent with septic embolic pneumonia. CT, computed tomography.



 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Download Citation
Download Citation Print
Print




